AHA Guidelines on Adult ECPR for VF/pVT/Asystole/PEA in the ACLS Manual
My connection to the AHA runs deep. I have had the pleasure of running two AHA training centers in Kuwait—MMI Kuwait Training Institute and the Prime Advanced Learning Institute. I thoroughly enjoyed working with people like Zehra' Al-Hilali, who headed up the AHA for the Middle East and North Africa region. Additionally, living in Kuwait was a wonderful experience that allowed me to immerse myself in a new culture and build lasting memories.
Now back in the USA, I recently completed my recertification for Basic Life Support (BLS) and Advanced Cardiovascular Life Support (ACLS); I was thrilled to find that the American Heart Association (AHA) has significantly expanded its coverage of Extracorporeal Cardiopulmonary Resuscitation (ECPR). What was once a brief mention has evolved into a comprehensive section dedicated to this critical intervention. As someone familiar with the AHA and its ACLS manual, I am excited to share this article, which summarizes the new ECPR guidelines. Additionally, I added some additional insights provided by the Extracorporeal Life Support Organization (ELSO).
ECPR Topics Covered in the AHA ACLS Manual
ECPR (Extracorporeal Cardiopulmonary Resuscitation) refers to venoarterial extracorporeal membrane oxygenation (ECMO) during cardiac arrest. ECPR techniques require adequate vascular access and specialized equipment. By using ECPR, providers can support vital organs with perfusion and gas exchange while reversible causes of cardiac arrest are addressed (e.g., acute coronary artery occlusion, pulmonary embolism, refractory ventricular fibrillation, profound hypothermia, cardiac injury, myocarditis, cardiomyopathy, congestive heart failure, drug intoxication). ECPR can also serve as a bridge for left ventricular (LV) assist device implantation or cardiac transplantation.
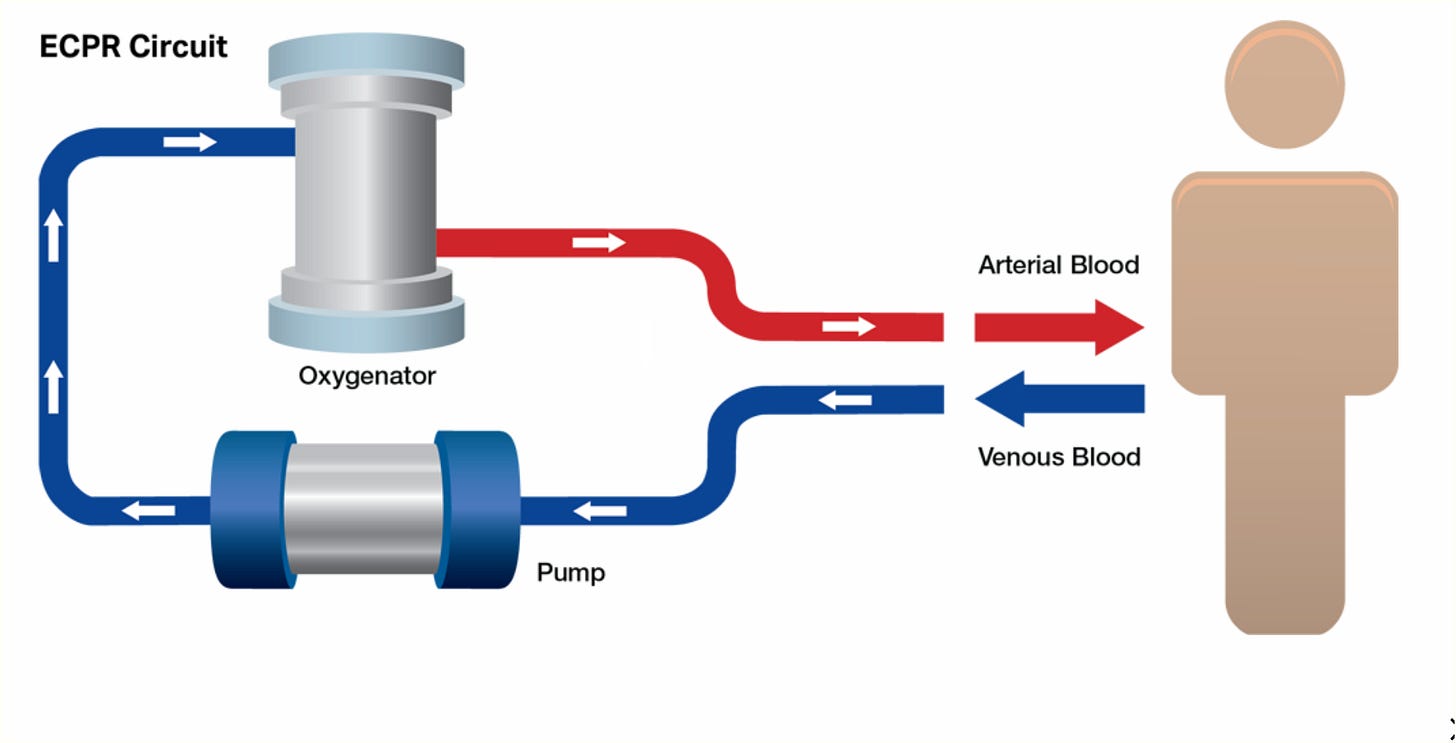
Components and Process: ECPR involves a venous cannula, a pump, and an oxygenator, providing temporary circulatory and respiratory support. This system can be rapidly deployed for patients with reversible causes of cardiac arrest when conventional Advanced Cardiovascular Life Support (ACLS) has failed.
Evidence and Benefits: ECPR has shown benefits in survival and neurologic outcomes compared to conventional CPR in patients with refractory cardiac arrest. However, its success relies heavily on timely intervention, appropriate patient selection, and specialized teams and equipment availability.
Indications for ECPR: ECPR is indicated for select patients experiencing cardiac arrest due to reversible causes, especially when conventional advanced cardiac life support (ACLS) measures have failed. Evidence suggests that ECPR can improve survival rates and neurological outcomes in specific scenarios.
Ventricular Assist Devices (VADs)
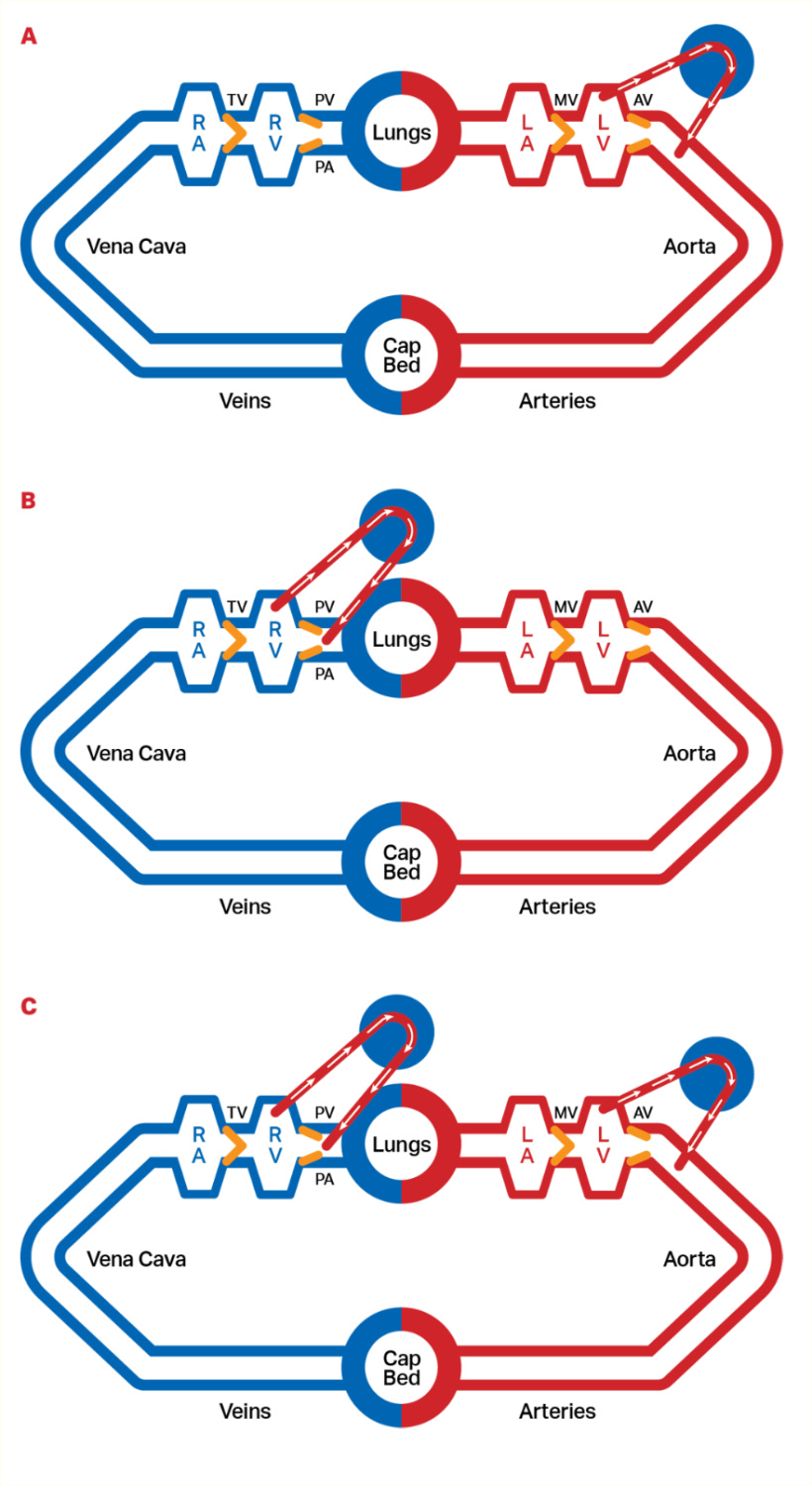
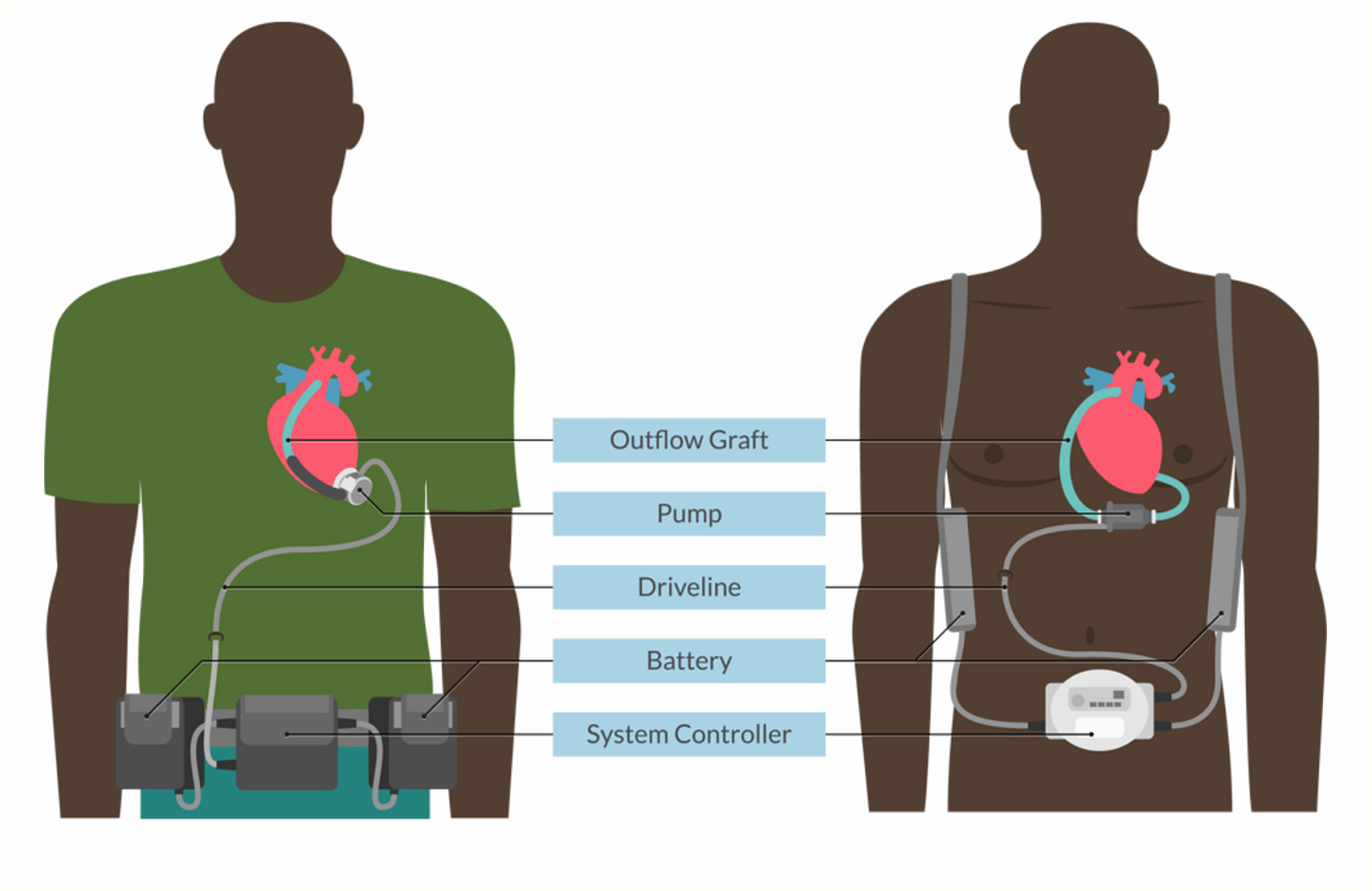
Definition and Purpose: Mechanical circulatory support devices, known as ventricular assist devices (VADs), support the function of the ventricles in patients with severe heart failure. These devices can be categorized based on the ventricle they support. Most VADs are implanted inside the thoracic or abdominal cavity.
Left Ventricular Assist Device (LVAD): Pumps blood from the left ventricle to the central aortic circulation.
Right Ventricular Assist Device (RVAD): This device pumps blood from the right ventricle or atrium to the pulmonary artery.
Biventricular Assist Device (BiVAD): Supports both ventricles.
Physiological Mechanisms: VADs can have different mechanisms, such as pulsatile-flow or continuous-flow devices. Due to their newer technology, continuous-flow devices are more commonly used.
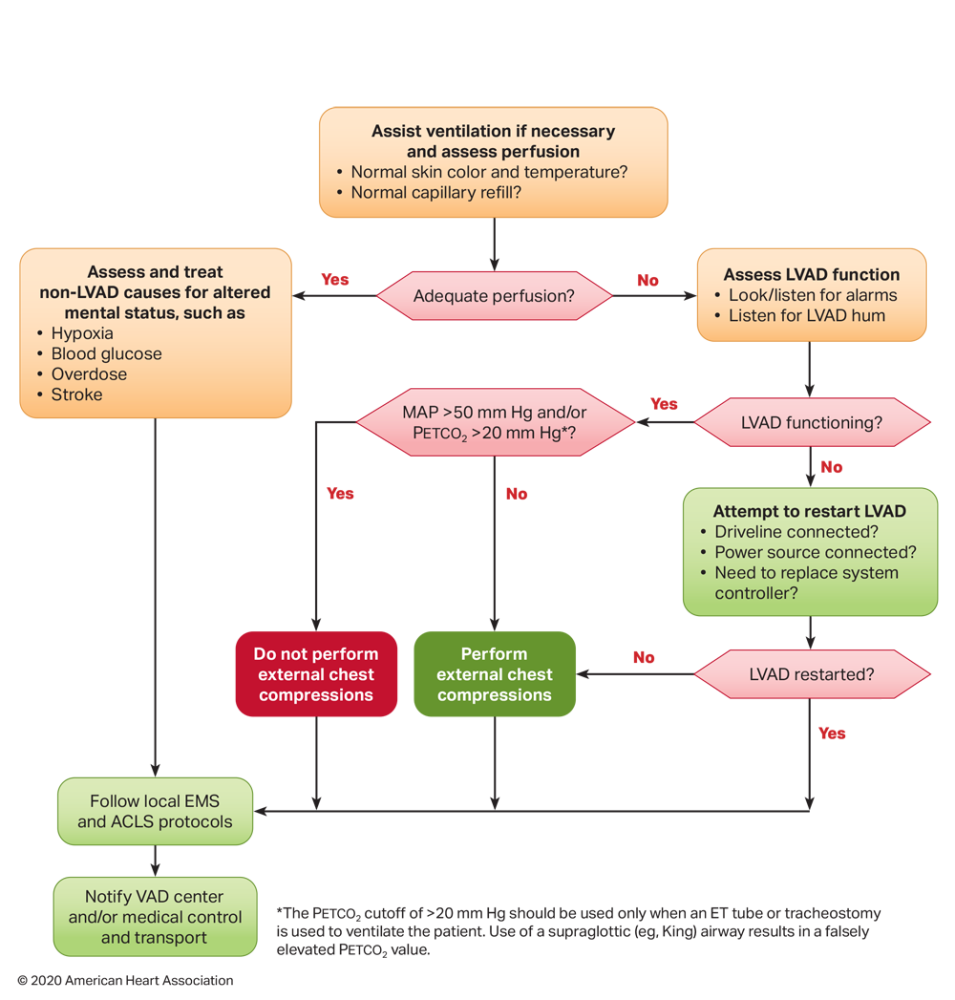
Management of VAD Patients: The management of patients with VADs involves ensuring proper function and connectivity of the device. A malfunctioning VAD could cause altered mental status or hypotension. So, it is important that the healthcare provider follows emergency protocols to quickly determine whether the signs and symptoms are coming from a malfunctioning VAD or from a non-VAD reason.
Emergency Response: EMS personnel must recognize the unique needs of VAD patients and ensure the VAD functions properly during resuscitation. They should check external pressure monitors, restart or manage VADs according to protocols, and identify VAD patients through medical alert devices or documentation.
Specific steps for emergency management include:
Assessing ventilation, oxygenation, and perfusion.
Checking the VAD function.
Checking for non-VAD causes of altered mental status, such as hypoxia, blood glucose, overdose, and stroke.
Ensuring the VAD is functioning correctly by checking alarms and listening for the VAD hum.
Restarting or managing the VAD if it malfunctions.
Following standardized protocols for VAD emergencies.
Special Considerations:
VAD patients may present with altered physical exam findings due to the continuous-flow nature of the devices.
Backup equipment and power sources are crucial for VAD patients.
Transporting VAD patients requires careful coordination to ensure device functionality and patient safety.
Hospital and Home:
Here is the AHA VAD Emergency Algorithm. Please spend some time looking at it.
Bonus: Topics ELSO addresses concerning ERCP Programs
Infrastructure and Equipment: An ECPR program requires significant investment in specialized ECMO equipment and dedicated space. Hospitals must have pumps, oxygenators, cannulas readily available and a designated area in the emergency department or cardiac catheterization lab for rapid ECPR initiation.
Personnel Training: A successful ECPR program requires a well-trained, multidisciplinary team. This team should include emergency physicians, intensivists, cardiac surgeons, and perfusionists who undergo regular simulations and skill maintenance sessions to ensure readiness for ECPR deployment.
Patient Selection Criteria: Clear protocols for identifying suitable ECPR candidates are crucial. These should include factors such as witnessed arrest, bystander CPR, and presenting rhythm, with rapid assessment tools to determine eligibility quickly and accurately.
Potential Complications: ELSO highlights specific complications associated with ECPR, such as vascular complications, neurologic injuries, and mechanical failures. Vigilant monitoring and rapid troubleshooting are essential to mitigate these risks and ensure continuous support.
Areas for Further Research that ELSO discusses:
Optimal Patient Selection: Refining criteria to identify patients most likely to benefit from ECPR is a critical area for investigation. This includes developing and validating predictive models for ECPR outcomes, which could help guide resource allocation and improve overall survival rates.
Timing of ECPR Initiation: Determining the optimal window for ECPR deployment is crucial for maximizing its effectiveness. Research comparing “ECPR first” strategies to conventional CPR approaches could provide valuable insights into the best way to use this resource-intensive intervention.
Long-term Outcomes: Assessing quality of life and functional status in ECPR survivors is essential for understanding the true impact of this intervention. Identifying factors associated with favorable long-term outcomes could help refine patient selection and post-ECPR care strategies.
To Sum it up
The AHA guidelines on ECPR now offer a detailed and structured approach for managing cardiac arrest in patients with refractory VF, pVT, asystole, or PEA. By integrating ECMO and VADs, these guidelines provide healthcare providers with the tools to deliver life-saving support, significantly improving patient outcomes. Proper management and continuous monitoring are crucial to the success of these advanced interventions.
References
Extracorporeal Life Support: The ELSO Red Book, 6th Edition. Published by the Extracorporeal Life Support Organization (ELSO), this comprehensive text is an important resource for understanding the principles and practices of ECMO.
ECMO Specialist Training Manual, 4th Edition. This manual provides in-depth training protocols and guidelines for ECMO specialists, covering cannulation techniques, patient management, and emergency procedures.
2020 American Heart Association Advanced Cardiovascular Life Support Provider Manual.
Various Other Source Materials. Additional insights and guidelines on ECMO practice, including hospital patient care practices.
Note: This article reflects my learning journey in ECMO and is intended for educational purposes only. It should not be used as a substitute for professional medical advice or guidance. Always consult with qualified healthcare professionals for clinical decisions and patient care.
Share and Subscribe. Join the ECMO 143 Learning Journey
Other Links:
Follow me on LinkedIn: Jonathan B. Jung, RRT-NPS
Follow me on X (Twitter) “ECMO 143-Stay Uptodate” List on X
Acknowledgments:
I developed three custom GPTs, “AI ECMO Expert,” “ECMO Specialist Handover Practice,” and “Micro Definitions (MD-GPT),” for specialized research. These tools draw primarily from the ELSO Redbook (6th Edition), the ELSO Specialist Training Manual (4th Edition), various research papers, and articles. Additional research was supported by GPT-4o/o1, Claude 3.5 Sonnet/Opus, and Perplexity. Editing was performed with Grammarly. A.I. images and charts were created using Leonardo AI, DALL-E3 AI Image Generator, Microsoft Designer, and Adobe Express. Content for all articles sourced from Extracorporeal Life Support: The ELSO Red Book, 6th Edition, and ECMO Specialist Training Manual, 4th Edition.


