Case Study: Refractory Metabolic Alkalosis
Guest Editors: Felipe de Andrade Arnaud, MD, PGY-5 Pulmonary and Critical Care Fellow, and Jeffrey M. Scott, DO FCCM E-AEC at the University of Miami/Jackson Memorial Hospital
I'm excited to introduce Dr. Felipe de Andrade Arnaud and Dr. Jeffrey M. Scott, who have graciously contributed to this newsletter edition as a guest editors. Their insights and dedication to advancing ECMO care are invaluable, and I deeply appreciate the time and effort they invested in presenting this case study. Their work exemplifies the critical thinking and expertise required in the complex pulmonary and critical care field.
Now, onto the case study presented by Dr. Arnaud and Dr Scott:
Introduction
A 35-year-old male with biventricular heart failure was undergoing evaluation for heart transplantation. The right heart catheter showed low cardiac output and elevated filling pressures, prompting Impella 5.5 placement as a bridge to transplant. Given further medical deterioration with RV failure and the need for multiple inotropes, the patient was then started on venoarterial extracorporeal membrane oxygenation (V-A ECMO) with drainage cannula in the right femoral vein and return cannula in the proximal left femoral artery.
Case Presentation
While on V-A ECMO, our patient developed a primary metabolic alkalosis with respiratory alkalosis per left radial arterial blood gas analysis revealing a pH of 7.58, PaCO2 of 39 mmHg, PaO2 of 111 mmHg, and bicarbonate (HCO3-) level of 37 mmol/L. It had been hypothesized that this was driven primarily by contraction alkalosis due to aggressive diuresis, and acetazolamide had been attempted with no improvement as well as a decrease on the ECMO sweep from 1 to 0.5 L/min to allow for greater CO2 retention, which should then minimize the alkalosis.
Still, contrary to expectations, worsening metabolic alkalosis was noted.

Management and Treatment
In response to the observed metabolic alkalosis, initial interventions were undertaken to promote bicarbonate excretion (via acetazolamide) or enhance CO2 retention (by decreasing the ECMO sweep). While physiologically justified, these measures proved ineffective due to the artificial nature of ECMO perfusion. The kidneys, responding to the sensed acidosis, increased the retention and production of bicarbonate. This created a vicious cycle; increasing CO2 retention and reduced bicarbonate availability would prompt further kidney bicarbonate retention with worsening alkalosis.
While clinical attention was focused on the systemic circulation, the actual cause of the metabolic alkalosis was identified in the post-oxygenation gas from the ECMO membrane, which demonstrated a respiratory acidosis (pH 7.27, PaCO2 97 mmHg, PaO2 409 mmHg, HCO3- 45 mmol/L). Given that the kidneys respond to acid-base disturbances based on multiple sensing mechanisms, they "sensed" the acidosis and retained bicarbonate to compensate, irrespective of the systemic acid-base status.
Outcome
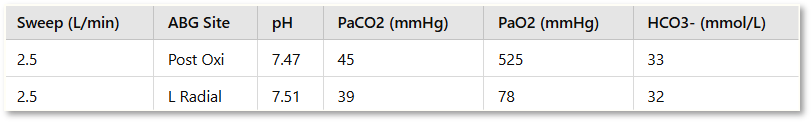
To break this cycle, it was imperative to recognize the concept of these different circulations and to redirect therapeutic efforts toward correcting the acid-base status at the renal level. Consequently, acetazolamide was discontinued, and the ECMO sweep was increased from 0.5 to 2.5 L/min. Follow-up arterial blood gas analysis performed 24 hours later demonstrated significant improvement: the left radial artery exhibited a pH of 7.51, PaCO2 of 39 mmHg, PaO2 of 78 mmHg, and HCO3- of 32 mmol/L; the ECMO post-oxygenation gas revealed a pH of 7.47, PaCO2 of 45 mmHg, PaO2 of 525 mmHg, and HCO3- of 33 mmol/L.

Discussion
An interesting acid-base phenomenon was hypothesized. The ECMO return cannula was positioned in the proximal femoral artery and directed retrograde (against the normal blood flow), creating a counter-flow towards the heart. This flow competes with the patient's native cardiac output, resulting in different body parts being perfused with blood with different acid-base profiles.
Blood ejected from the heart (anterograde) represents the systemic acid-base status recognized by the central nervous system (CNS) and its respiratory centers. This circulation is used to monitor the pH and to achieve optimal environments for metabolic and pharmacologic reactions, to ensure equilibrium of biochemical processes, protein structures, and even oxygen delivery to tissues.
Conversely, the blood reinfused from the ECMO circuit, retrograde through the femoral artery, mirrors the acid-base environment created by the ECMO post membrane environment, designed solely to address the systemic circulation's requirements. The mixing point between these two circulations can vary depending on native cardiac output, with higher outputs resulting in a mixing cloud further from the aortic arch.
This differential perfusion could lead to an interesting clinical condition if the mixing cloud is situated above the level of the renal arteries. In such a scenario, a discrepancy arises between the acid-base disturbance recognized by the kidneys (reflecting ECMO output) and that perceived by the CNS (reflecting native output), potentially resulting in opposing compensatory mechanisms. In this patient, the left radial artery was perfused by the native cardiac output, while the ECMO current supplied the renal arteries.
It is worth mentioning that in a usual configuration, a right radial arterial line is preferred due to its origin in the brachiocephalic trunk, which helps to monitor for the occurrence of Harlequin syndrome, among other uses. In this patient, the left radial artery was found to be anatomically more favorable for cannulation, and therefore, it was utilized with no significant detriment in this particular case.
In patients with heart failure, previous studies have demonstrated that metabolic alkalosis is associated with reduced myocardial contractility, the occurrence of arrhythmias, decreased cerebral blood flow, and impaired peripheral oxygen unloading. Furthermore, metabolic alkalosis has been identified as an independent risk factor for in-hospital mortality in this patient population.
Conclusion
The utilization of extracorporeal membrane oxygenation (ECMO) is experiencing significant growth, accompanied by both emerging challenges and discoveries. Given the critical importance of expertise in enhancing our understanding of this complex therapy, we aim to highlight this compelling example and disseminate it widely.
The phenomenon described in this case, differential gas exchange, has recently gained attention and remains unfamiliar to many specialists. Furthermore, recent examinations indicate that the Extracorporeal Life Support Organization (ELSO) still needs to address this topic. Consequently, our initiative aims to advance collective knowledge and equip healthcare professionals to tackle challenges and enhance patient outcomes.
Closing Remarks
Again, thank you to Dr. Felipe de Andrade Arnaud and Dr. Jeffrey M. Scott for contributing as a guest editor for this newsletter edition. Their deep understanding of critical care and ECMO management has provided valuable insights into the complexities of acid-base disturbances during ECMO. I hope this case sparks further discussion and learning among our readers as we continue to explore the evolving landscape of ECMO.
As always, I encourage any questions or comments and look forward to sharing more expert contributions in future editions.
Join the ECMO 143 Learning Journey
Note: This article is intended for educational purposes only. It should not be used as a substitute for professional medical advice or guidance. Always consult with qualified healthcare professionals for clinical decisions and patient care.
Other Links:
https://bit.ly/ecmo143-youtube
https://bit.ly/ecmo143-fbgroup
https://bit.ly/ecmo143-company
Acknowledgments:
Here is a list of tools and resources that assisted in creating this article and others. I developed three custom GPTs to assist in specialized research: AI ECMO Expert, ECMO Specialist Handover Practice, and Micro Definitions (MD-GPT). These tools were instrumental in gathering and analyzing information from key sources.
Special thanks to the AI platforms and tools that facilitated this research:
GPT-4o/o1, Claude 3.5 Sonnet/Opus, Perplexity
Grammarly for editorial and proofreading assistance
Leonardo AI, DALL-E3 AI Image Generator, Microsoft Designer, and Adobe Express for generating images and visual content