🫁 David’s Long Battle: A Survivor’s Journey Through ECMO and Beyond
Key Points:
David Richards was a healthy 48-year-old when swine flu triggered a cascade of critical illness.
Within days, he developed severe ARDS and was placed on ECMO at Glenfield Hospital in the UK.
Complications, including bleeding and pneumothorax, nearly ended his life.
His recovery included weeks of coma, vivid hallucinations, and grueling physical rehab.
More than a decade later, David still lives with the long-term effects—but also with deep gratitude.
In late 2009, David Richards caught what seemed like a typical seasonal flu. He called in sick to work on Friday, November 27, thinking he’d be back by Monday.
He never returned.
Over the next two weeks, his symptoms worsened. He called his GP three times, describing crushing fatigue and breathlessness. Each time, he was told to drink fluids, take paracetamol, and rest. But his condition spiraled. A friend who was with him remembers hearing him say on the phone, “Please help me—I feel like I’m dying.”
He wasn’t exaggerating.
A Sudden Collapse
When David stopped answering calls, his parents, 150 miles away, drove to check on him. They found him incoherent, barely breathing. Paramedics rushed him to Gloucestershire Royal Hospital, where he was placed in a medically induced coma and ventilated. He had developed ARDS (Acute Respiratory Distress Syndrome), a life-threatening condition where fluid fills the lungs, blocking oxygen from entering the blood.
Despite prone positioning and maximum ventilator settings, David’s oxygen levels continued to drop. His local ICU team had exhausted all options.
The Call to Glenfield
Glenfield Hospital in Leicester—then the UK’s only adult respiratory ECMO center—was contacted. With only five ECMO beds, placement was rare. But David was accepted. A mobile retrieval team arrived with ECMO equipment, placed him on the circuit bedside, and transported him under police escort.
“He had three hurdles,” the consultant told David’s family. “Survive the transfer. Survive cannulation. And survive the complications of ECMO itself.”

The Fight for Survival
Connected to ECMO, David’s blood was now oxygenated outside his body. His lungs could rest.
But survival wasn’t guaranteed.
He developed a double pneumothorax. A tracheostomy was performed. And then came the bleeding—persistent hemorrhaging from his neck and chest tubes. At one point, he was losing 300ml of blood every 90 minutes, despite multiple transfusions.
Eventually, ECMO had to be discontinued. Miraculously, his lungs had recovered enough to function with ventilator support alone. He was transferred back to Gloucestershire Royal ICU—still unconscious, unaware of how close he had come to death.

Waking Up in a Different World
When David began to regain consciousness, nothing made sense.
In his mind, he’d been living in a dream—except it wasn’t peaceful. It was terrifying. He believed he’d been shot. That his daughters were kidnapped. That he was dying all over again.
These were ICU hallucinations, a form of ICU delirium common in long-term sedation. But they felt real.
What helped anchor him was an ICU diary kept by the mother of his baby son and his parents. It chronicled phone calls, procedures, daily updates, and simple words of love. That diary became his map back to reality.
“It helped me filter out the false memories and piece together what actually happened,” he wrote.
Communication and Rehab: Starting from Zero
Physically, David was starting from scratch. He couldn’t speak due to his trach. Early attempts to write or use an alphabet board were frustrating and exhausting. Even holding a phone was impossible.
Eventually, a Passy-Muir valve allowed him to speak—weakly and only for a few minutes at a time. But it was a start.
Rehab began with simple movements: lifting his foot, and rotating his ankle. A former athlete, David had pushed through pain before—but nothing like this.
“I’ve sprinted until I threw up. But trying to sit up in bed was another level.”
Discharge: But Not the End
Two weeks after returning from Glenfield, David was weaned off the ventilator. His trach and feeding tube were removed. He transitioned to the respiratory ward, still in a wheelchair.
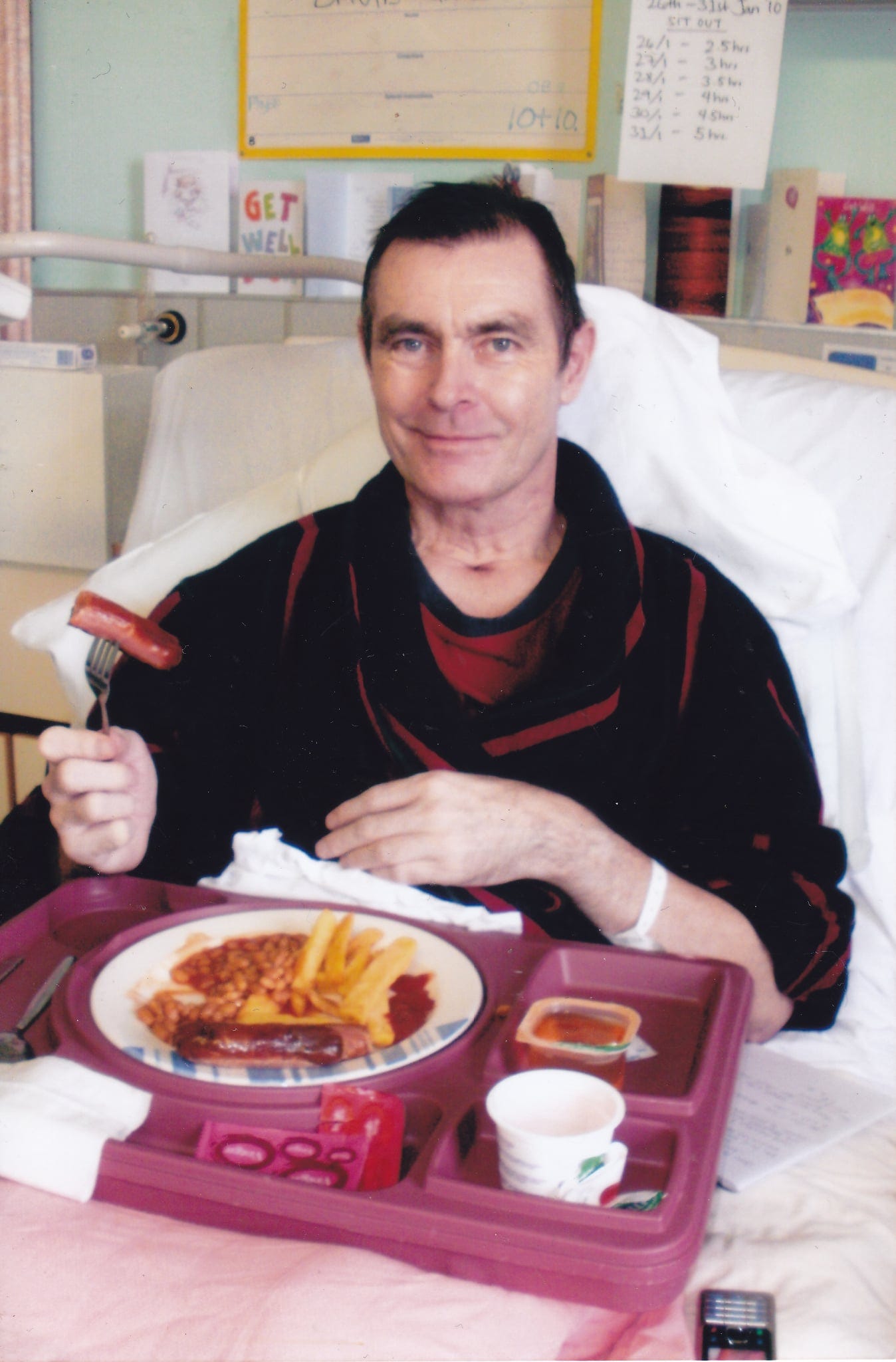
His first real meal in nearly two months—sausage, beans, and chips—was photographed to mark the occasion.
Eventually, he stood. Then shuffled with a walker. His daughters pushed him to the shop in a wheelchair. It took eight months before he could set the wheelchair aside for good.
Life After ICU
Going home was not a victory lap. It was the beginning of a new struggle.
David joined outpatient rehab, eventually spending over 2.5 years in various programs. He battled fatigue, joint pain, short-term memory loss, and crushing disappointment. His career in defense and intelligence—nearly 30 years—ended in medical retirement at age 49.
He was also diagnosed with PTSD. The nightmares persisted. He underwent CBT and then EMDR therapy, which finally helped him cope.
The Long View
Years later, David returned to Glenfield to thank the team that saved him. He stood in front of the ECMO machine, which gave him time to heal.
“My son was four months old when I got sick. He’s now twelve. And he has a father in his life because of ECMO. That’s the bottom line.”
Takeaway
ECMO doesn’t just save lives—it gives people the chance to live again. But survival is only part of the story. The emotional, physical, and financial toll of recovery is real, long-lasting, and often invisible.
David’s journey reminds us that every ECMO survivor walks a road few can understand—but one worth walking.
Postscript (From David Richards):
After reading this article, David shared that Glenfield Hospital had a reciprocal arrangement with Karolinska University Hospital in Sweden prior to 2009, allowing patients to be flown between the two when ECMO beds were full. He considers himself incredibly fortunate to have received a bed in time. His survival—along with others during the 2009 and 2010 swine flu waves—helped influence the creation of a centrally funded regional network of adult respiratory ECMO centers in England.
Thanks for reading ECMO 143: A Patient & Family Guide! Subscribe for free to receive new posts and support my work.