ECMO Circuit Management: Insights from the ELSO Red Book and ECMO Specialist Training Manual
Effective ECMO circuit management is critical for patient safety and optimal outcomes, as the Extracorporeal Life Support Organization (ELSO) guidelines emphasize. Maintaining a well-functioning ECMO circuit requires diligence and a multidisciplinary approach, from proactive surveillance to fluid management and infection control. This article outlines key recommendations from ELSO’s Red Book and Training Manual on circuit management, focusing on best practices and early intervention strategies.
Proactive Circuit Surveillance
Routine and meticulous examination of the ECMO circuit is paramount. ELSO guidelines recommend a structured approach to these checks, as even minor issues can escalate quickly if not addressed.
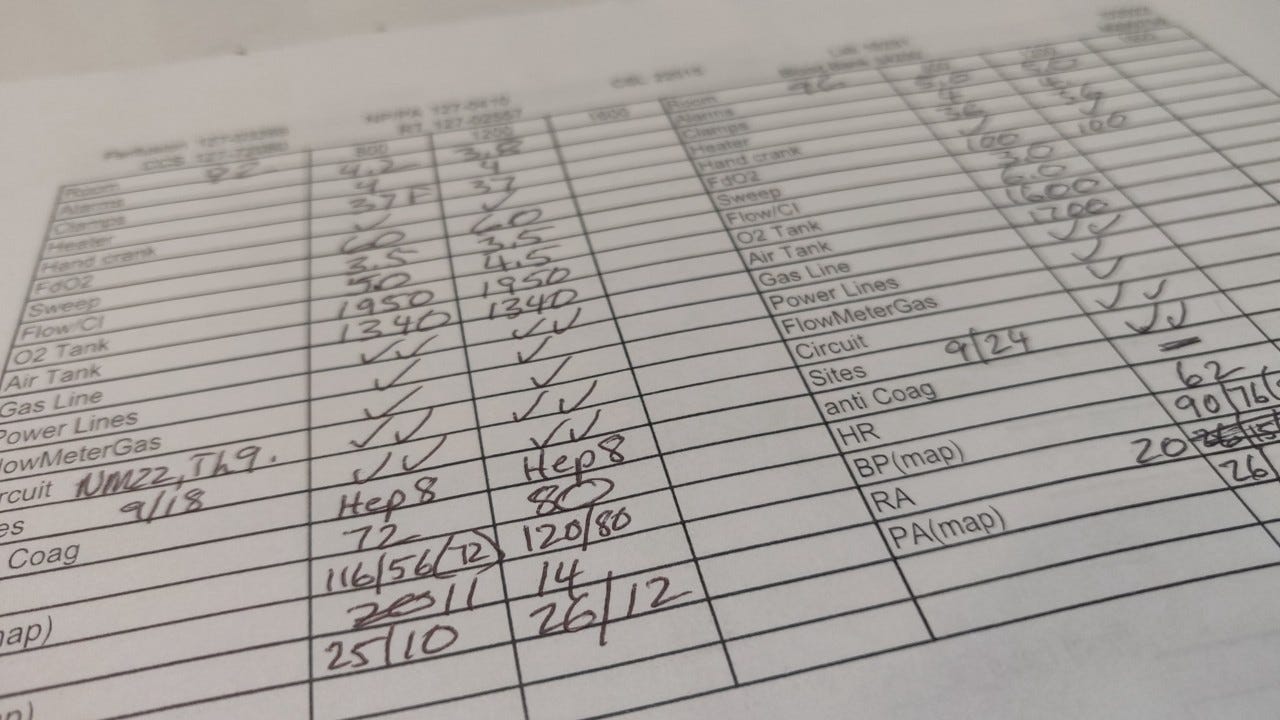
Throughout my various careers—whether as a news video editor, quick lube manager, respiratory therapist, training center director, or project manager—I have always relied on checklists to stay organized and avoid mistakes or forgetting something. While I can’t recall which college class introduced me to the concept, the importance of checklists has been evident in every role I’ve held. Originally developed in aviation during the mid-20th century to reduce errors, checklists have since been adapted to healthcare, as highlighted in Atul Gawande’s “The Checklist Manifesto.” For ECMO specialists, checklists are invaluable, allowing us to focus on the complexities of patient care while ensuring that critical circuit checks are never overlooked. I will use my checklist in the patient’s room and transfer the information into the EMR.
Frequency: Circuit checks should be performed at the start of each shift and repeated hourly. This routine assessment ensures that subtle changes are caught early and promptly addressed.
Scope: A comprehensive circuit check includes: Inspecting all plugs and fluid connectors for secure connections.Verifying that alarms are set appropriately and functioning correctly.Examining tubing for color changes, kinks, or any signs of damage.Documenting parameters like RPM, flow rate, sweep gas flow, FiO2, and circuit pressures.Checking the oxygenator and tubing for clots or fibrin deposition, using a high-intensity flashlight to aid visualization.
In my experience, I’ve seen how minor malfunctions, such as oxygen gas lines popping off or air entrainment during medication infusions, can occur unexpectedly. Fortunately, vigilant circuit checks—supported by a checklist—have allowed me to catch these issues early and correct them before they escalate. These incidents underscore the importance of being present and alert when managing ECMO circuits. Quick intervention can prevent a potentially serious situation, whether it’s a pigtail detaching from the oxygenator or air entering the circuit due to a missing filter. Regular checks and constant vigilance are crucial to ensuring patient safety.
Early Detection of Clot Formation
Clot formation is a significant risk in ECMO, making vigilance key to early detection and management:
Transmembrane Pressure Trends: Monitor for gradual increases in transmembrane pressure, even without changes in gas exchange, as this can signal early clot formation.
Gas Exchange Parameters: Decreases in the pre- and post-oxygenator PaO2 differential or a drop in oxygen saturation can also indicate clot burden.
Visual Inspection: Regular visual examination of the oxygenator and tubing is crucial. The fibrin deposition, often seen as white strands or a milky appearance in the tubing, warrants immediate attention.
Collaboration and Intervention: Any suspicion of clotting requires immediate consultation with the perfusion team to determine if a membrane lung or complete circuit change is necessary.
Fluid Management Expertise
ECMO specialists play a crucial role in managing fluid balance since these patients are susceptible to acute kidney injury (AKI) and fluid overload:
Recognizing “Chugging”: Frequent volume infusions to maintain ECMO flow, often called “chugging,” may indicate inadequate intravascular volume in an ECMO circuit. Early recognition and reporting can guide appropriate management.
Fluid Goal: Collaborating closely with the care team ensures that fluid administration or removal is aligned with the patient’s clinical goals.
Circuit Integration for Fluid Removal: Understanding how to integrate devices like continuous renal replacement therapy (CRRT) or a hemoconcentration into the ECMO circuit is essential for effective fluid management.
Infection Control
Maintaining a sterile ECMO circuit is vital to prevent infections, which can have serious consequences:
Minimizing Access Points: Reducing the number of times the circuit is accessed for blood draws or medication administration lowers contamination risk.
Securing Stopcocks: Ensure all unused stopcock ports have dead-end caps, ideally alcohol-impregnated, to reduce bacterial entry.
Meticulous Cleansing: Always clean circuit access points with alcohol before and after use.
Collaborative Cannula Care: Work closely with nurses to ensure proper cannula care, including daily checks for secure holders, stitches, and clean insertion sites.
Heater-Cooler Device Maintenance: Adhere to strict maintenance and positioning protocols for HCDs connected to the ECMO circuit, as these devices have been linked to infection outbreaks.
So.......
Specialists can enhance patient safety and improve outcomes by following these critical ECMO circuit management practices. Continuous learning, collaboration, and adherence to established guidelines are the cornerstones of excellence in ECMO care. Feel free to share your insights or questions on ECMO circuit management in the comments below!
Share and Subscribe. Join the ECMO 143 Learning Journey
Other Links:
Follow me on LinkedIn: Jonathan B. Jung, RRT-NPS
Follow me on X (Twitter) “ECMO 143-Stay Uptodate” List on X
Acknowledgments:
I developed three custom GPTs, “AI ECMO Expert,” “ECMO Specialist Handover Practice,” and “Micro Definitions (MD-GPT),” for specialized research. These tools draw primarily from the ELSO Redbook (6th Edition), the ELSO Specialist Training Manual (4th Edition), various research papers, and articles. Additional research was supported by GPT-4o/o1, Claude 3.5 Sonnet/Opus, and Perplexity. Editing was performed with Grammarly. A.I. images and charts were created using Leonardo AI, DALL-E3 AI Image Generator, Microsoft Designer, and Adobe Express. Content for all articles sourced from Extracorporeal Life Support: The ELSO Red Book, 6th Edition, and ECMO Specialist Training Manual, 4th Edition.