Mobilizing ECMO Patients for Recovery
By Dr. David Jergenson, DPT Physical Therapist – Cardiac Lead, Mayo Clinic, Rochester, MN
Guest Editor: Dr. David Jergenson, DPT, a physical therapist at Mayo Clinic in Rochester, MN
In ECMO care, we focus heavily on hemodynamics and oxygenation, but recovery extends beyond the circuit. Early mobilization is key in reducing delirium, shortening hospital stays, and restoring independence, yet it comes with unique challenges.
This week’s guest editor, Dr. David Jergenson, DPT, a physical therapist at Mayo Clinic in Rochester, MN, shares his insights on safely mobilizing ECMO patients. He discusses the barriers, strategies, and interdisciplinary collaboration needed to make movement possible.
Let’s explore how mobilization can transform ECMO recovery:
Like so many in the inpatient population, there are countless benefits to patients on ECMO mobilizing. Not only do patients get stronger, but it also helps reduce delirium, decreasing length of stay and undoubtedly provides hope for the critically ill. As a physical therapist, it’s my job to make it happen.
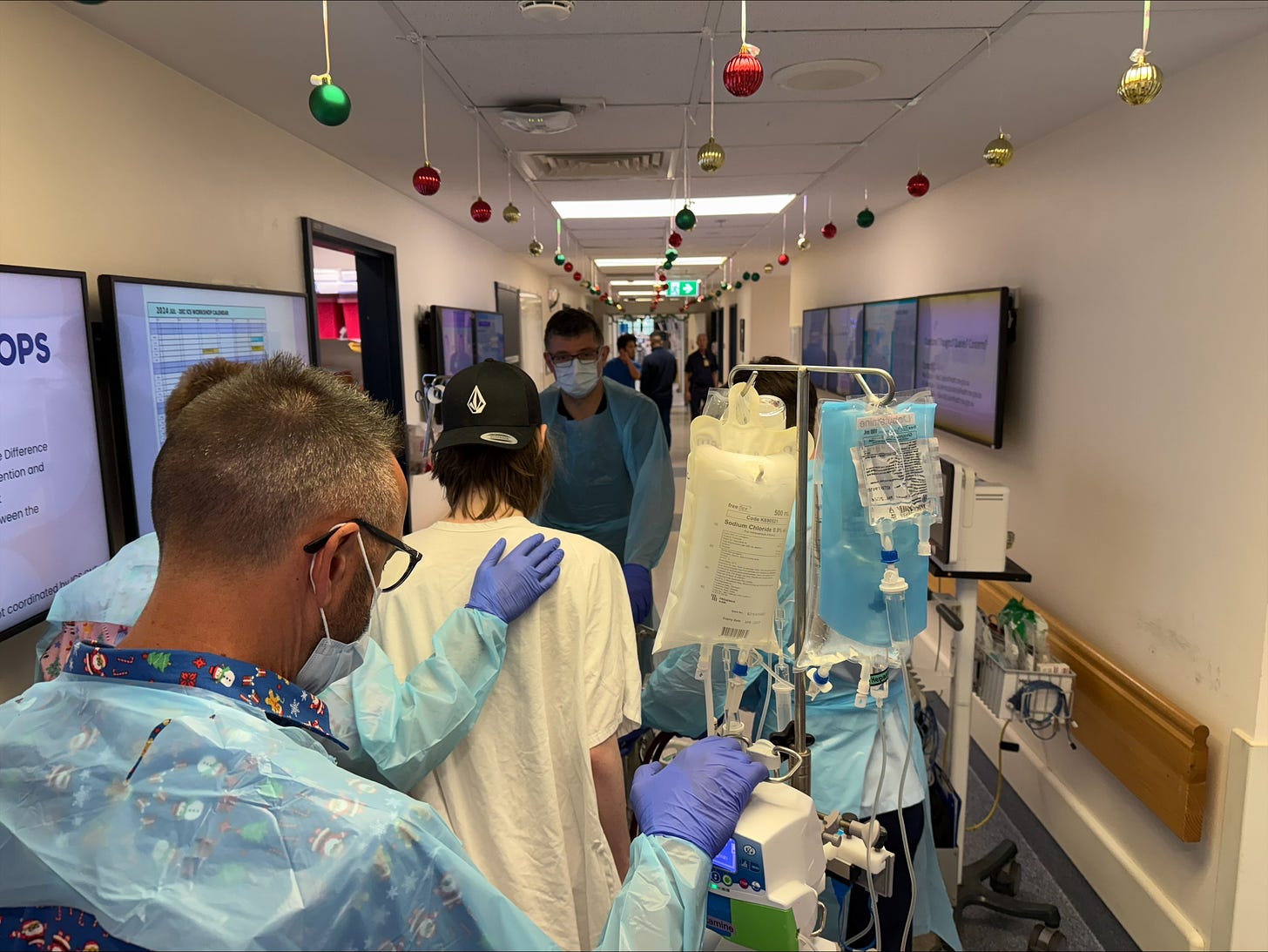
Patient abilities can vary due to their strength, cognition, hemodynamics, or all of the above, and rates of ICU-acquired weakness in ECMO patients are often higher than those of the general ICU population. Some patients are so debilitated that we focus on sitting balance or performing sit-to-stand exercises for several weeks. If the patient cannot take steps, we sometimes use a ceiling lift or Sara Stedy device to transfer a patient to a chair. Others have the strength to ambulate several hundred feet! Each patient's ECMO journey is unique. Some had complicated cardiac surgery. Others are awaiting heart and/or lung transplants. Regardless of their differences in background and complexity, the goals of returning to independence remain the same.

The Power of Movement in ECMO Recovery
Studies have shown that mobilizing patients on ECMO is overall safe. As with all mobility, risks are always involved, but the benefits far outweigh the low chance of harm. At my facility, we frequently mobilize patients with various cannulation strategies and support (VA, VV, VAV, etc.). There used to be a previous thought that patients who were femorally cannulated needed to be on bedrest; we frequently mobilize these patients and have not had any major adverse events. For these patients, flexing the hip to 90 degrees on the cannulated side while supine helps assess whether ECMO flows change in a seated position.
Interdisciplinary communication is vital for success in mobilizing ECMO patients. There is frequent dialogue regarding line management and patient response to activity between the critical care team, PT, OT, nursing, and the ECMO specialist. The ECMO specialist sometimes increases the FiO2 or sweep to improve patient symptoms or hemodynamics. These changes are documented in our therapy notes for reference in future sessions. We also mobilize patients whose sweep gas is clamped on ECMO, as their activity tolerance can help determine decannulation readiness. The journey for these patients can be very challenging, but the mobility team is undoubtedly integral to recovery.
Sources: Abrams, D., Madahar, P., Eckhardt, C. M., Short, B., Yip, N. H., Parekh, M., Serra, A., Dubois, R. L., Saleem, D., Agerstrand, C., Scala, P., Benvenuto, L., Arcasoy, S. M., Sonett, J. R., Takeda, K., Meier, A., Beck, J., Ryan, P., Fan, E., Hodgson, C. L. (2022). Early Mobilization during Extracorporeal Membrane Oxygenation for Cardiopulmonary Failure in Adults: Factors Associated with Intensity of Treatment. Annals of the American Thoracic Society, 19(1), 90–98. https://doi.org/10.1513/AnnalsATS.202102-151OC
Chatziefstratiou, A. A., Fotos, N. V., Giakoumidakis, K., & Brokalaki, H. (2023). The Early Mobilization of Patients on Extracorporeal Membrane Oxygenation: A Systematic Review. Nursing reports (Pavia, Italy), 13(2), 751–764. https://doi.org/10.3390/nursrep13020066
Chen, X., Lei, X., Xu, X., Zhou, Y., & Huang, M. (2022). Intensive Care Unit-Acquired Weakness in Patients With Extracorporeal Membrane Oxygenation Support: Frequency and Clinical Characteristics. Frontiers in medicine, 9, 792201. https://doi.org/10.3389/fmed.2022.792201
Note: This article is intended for educational purposes only. It should not be used as a substitute for professional medical advice or guidance. Always consult with qualified healthcare professionals for clinical decisions and patient care