TEG: Watching the Life of a Clot in Real Time
🗓️ This is an advanced release from my LinkedIn newsletter. The full article goes live on LinkedIn at 7:30 AM tomorrow.
Key Points:
Traditional coagulation tests provide static snapshots; TEG offers a dynamic, real-time assessment of clot formation and breakdown.
TEG parameters—R time, K time, alpha angle, MA, and LY30—provide insights into different phases of coagulation and fibrinolysis.
Heparinase-modified TEG helps differentiate between heparin effect and intrinsic coagulopathy.
Simultaneous standard and heparinase TEG assays are essential for accurate interpretation in patients on heparin therapy.
I used to think I understood TEG. Then a nurse asked me to explain it, and I was trying to make sense of it as I was explaining it. I knew the R time had something to do with when the clot starts, and MA was the widest part of the graph, but beyond that? Blank.
So, I did what any good ECMO Specialist would do: I went home, pulled out my notes, rewatched some TEG videos, and realized something that changed everything:
Labs like PT, INR, fibrinogen, aPTT, platelets, and anti-Xa are snapshots. But TEG is a movie.
It doesn’t just tell you what’s in the blood. It shows you what the blood can do, from the moment fibrin starts to form to when the clot breaks down. For ECMO patients, especially those receiving multiple blood products, undergoing trauma resuscitation, or living on the edge of DIC, TEG offers a dynamic look at coagulation in real time.
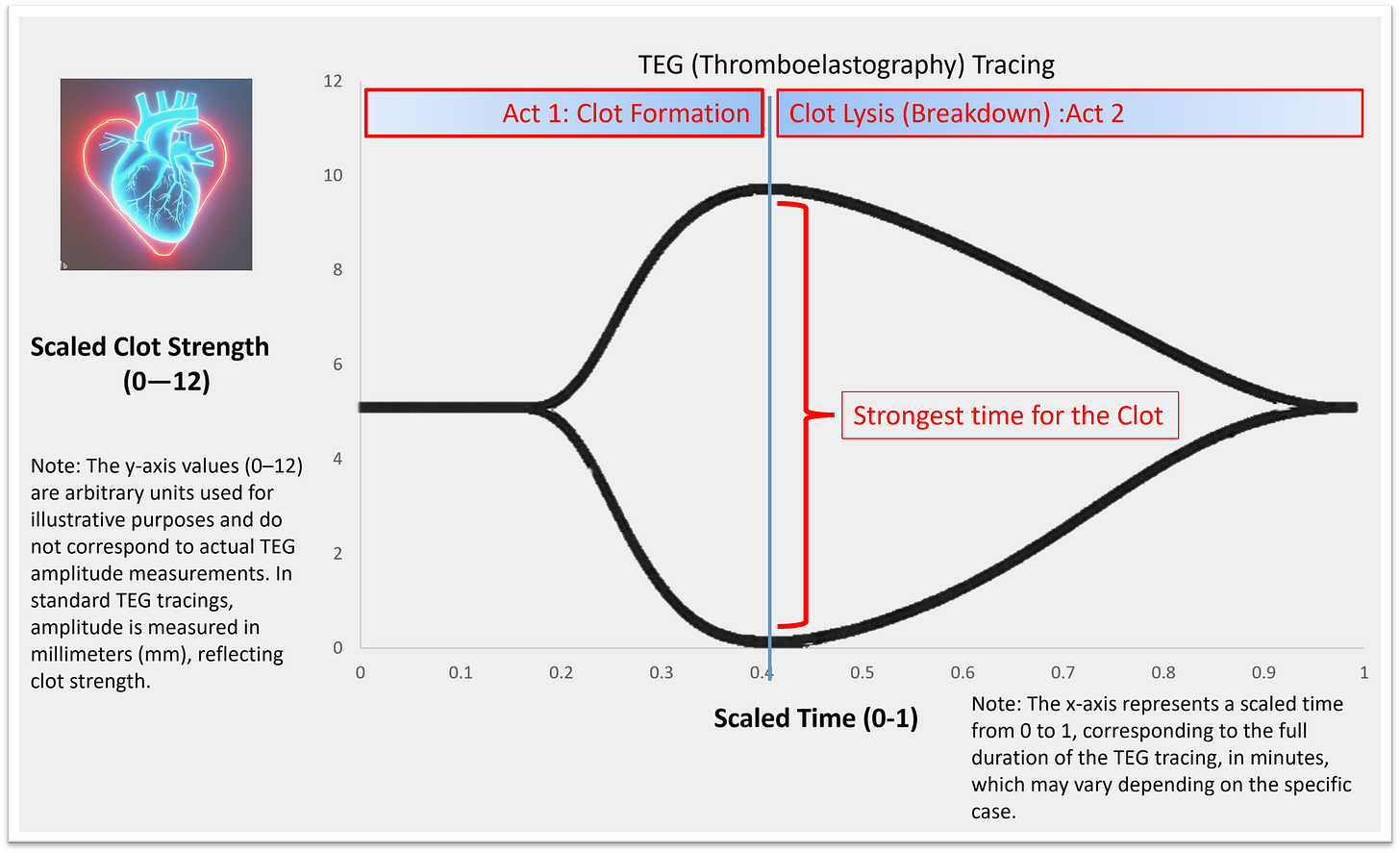
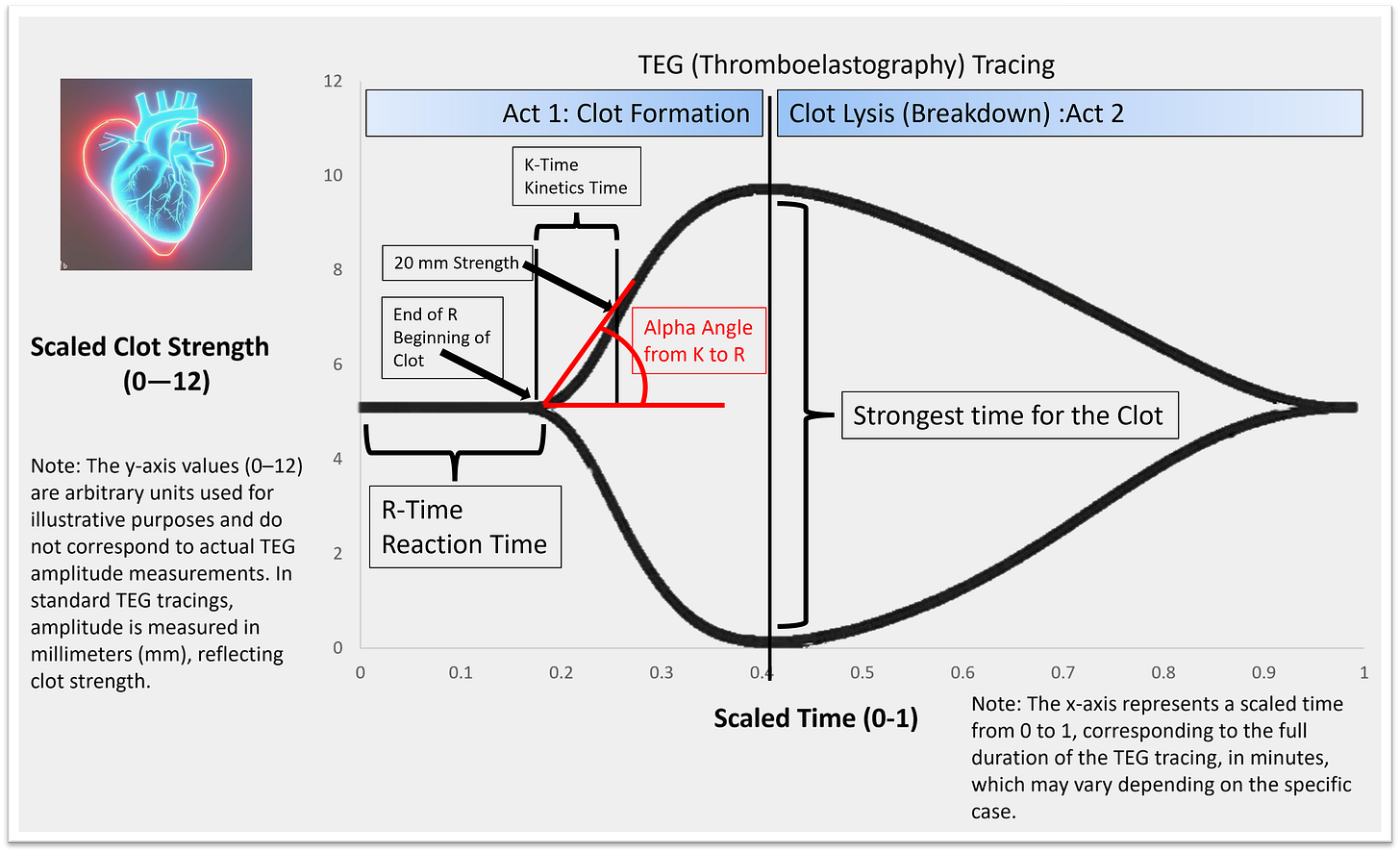
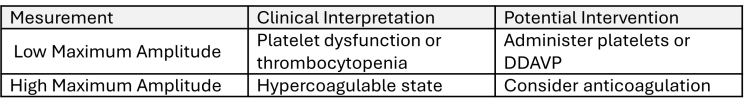
Two Halves of the TEG Story
Think of the TEG tracing as the lifespan of a clot, split into two acts:
Act 1: Clot formation (Coagulation)
Act 2: Clot breakdown (Fibrinolysis)
The X-axis is time. The Y-axis is the strength of the clot, measured by the movement of a pin suspended in the blood sample.
The standard test takes about 30–60 minutes, but Rapid TEG compresses it into 15 minutes—ideal in trauma, surgery, or acute ECMO changes.
TEG Parameters Explained
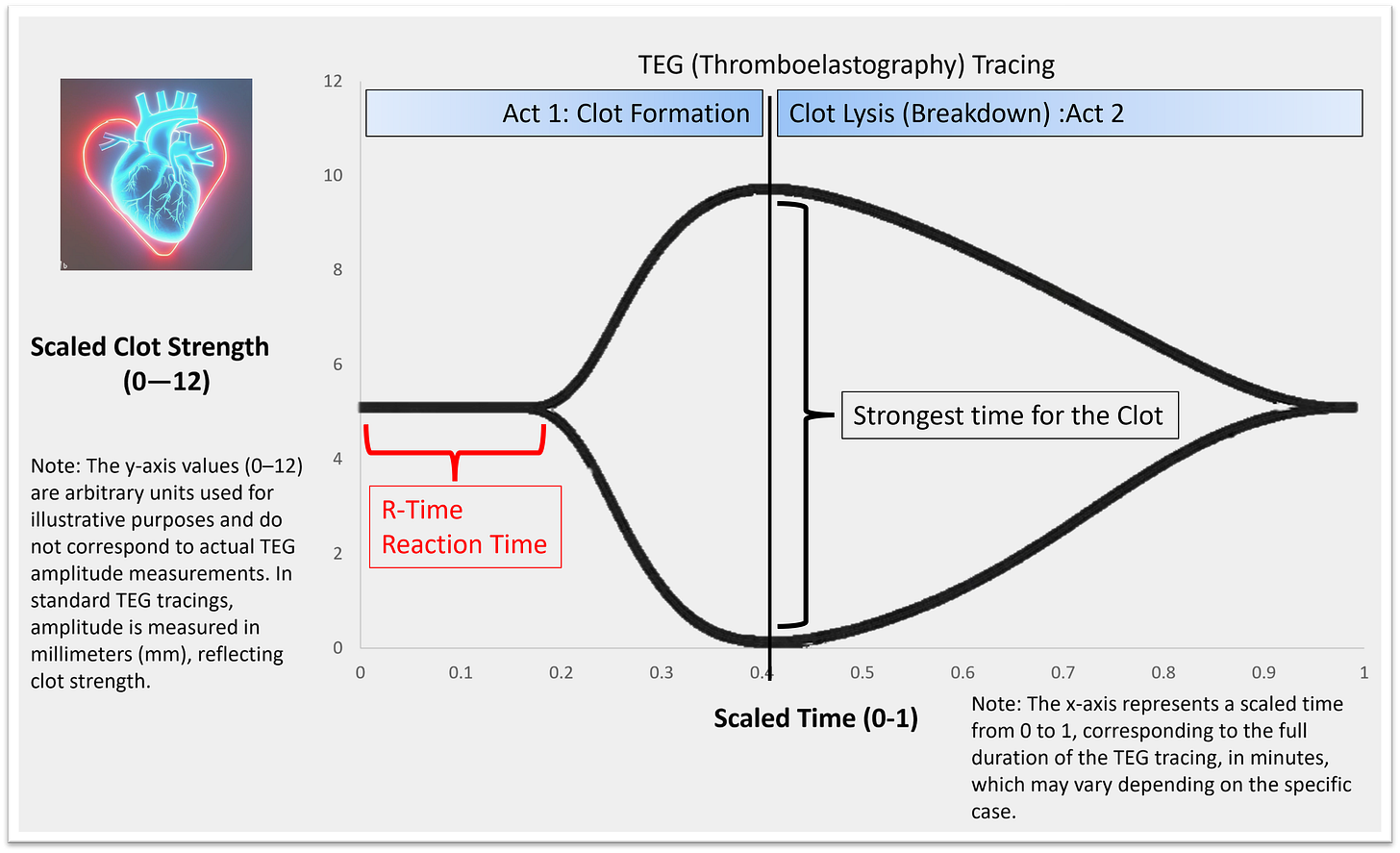
R Time (Reaction Time)
What it measures: Time to initial fibrin formation
Reflects: Coagulation factor levels and thrombin generation
Normal Range: 4–8 minutes
Interpretation/Intervention:
Tip: Always check a heparinase TEG if R is prolonged. It helps separate drug effect from true deficiency.
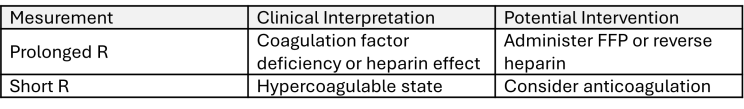
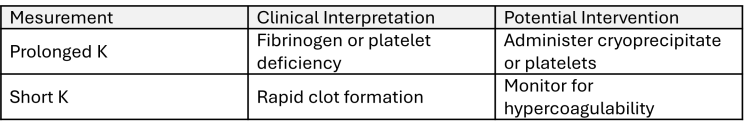
K Time (Kinetics)
What it measures: Time from R to reach 20 mm clot strength (speed in time it took to get to 20mm clot strength)
Reflects: Fibrinogen and platelet interaction
Normal Range: 1–4 minutes
Interpretation/Intervention:
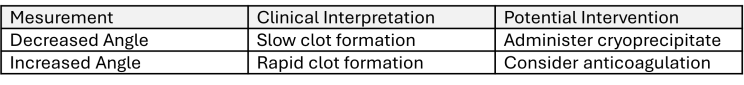
Alpha Angle (α)
What it measures: Slope between R and 20 mm clot strength (speed to get to 20mm clot strength)
Reflects: Speed of clot formation
Normal Range: 47–74 degrees
Interpretation/Intervention:
Note: K time and alpha angle are interrelated; abnormalities in one often reflect in the other.
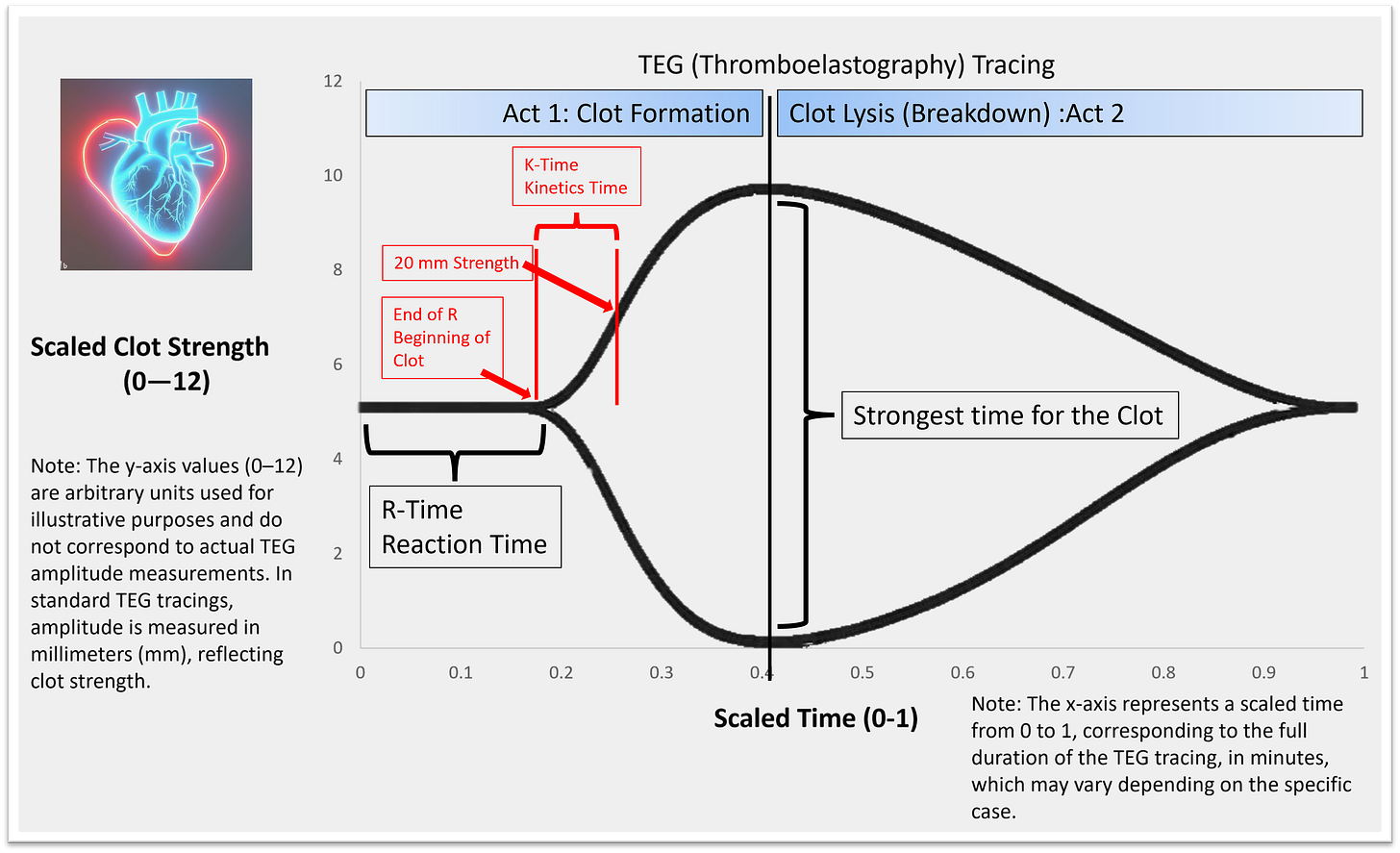
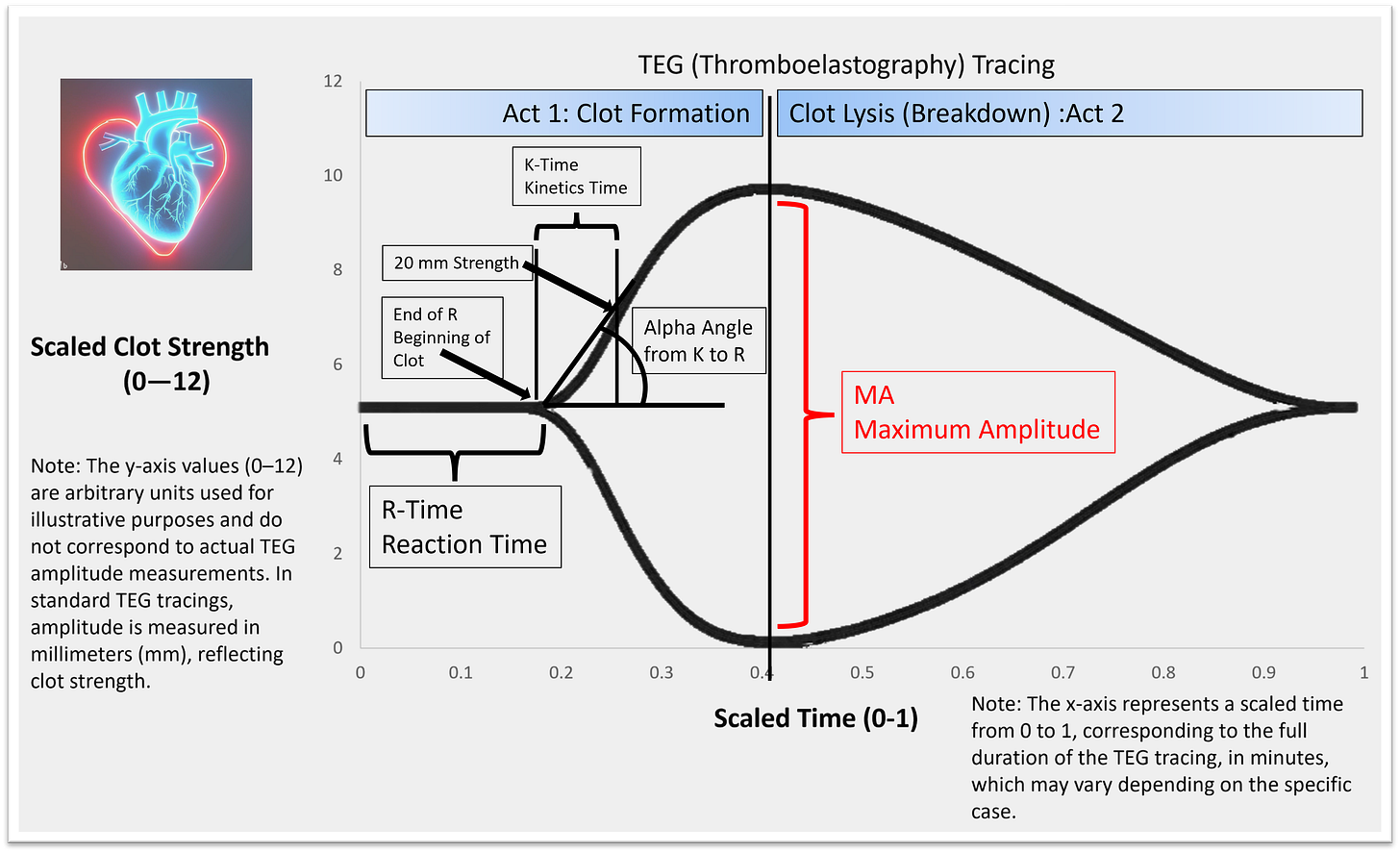
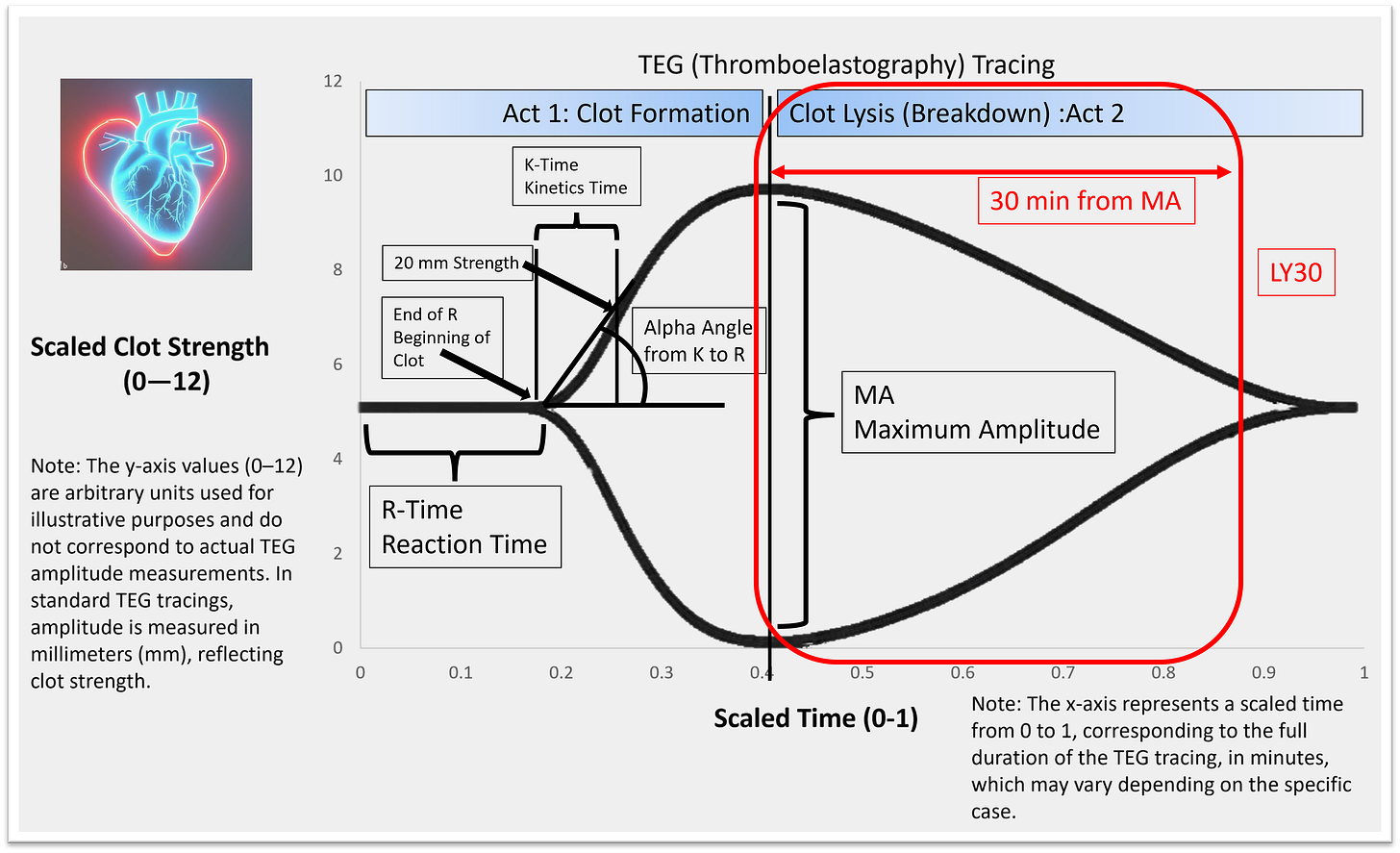
Maximum Amplitude (MA)
What it measures: The strongest point of the clot
Reflects: Platelet number and function
Normal Range: 55–73 mm
Interpretation/Intervention:
Everything to the left of the MA is about building the clot. Everything to the right is about breaking it down.
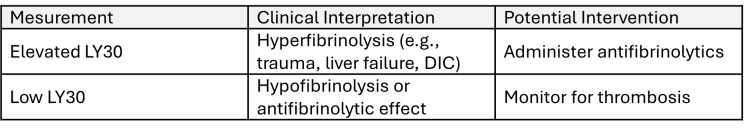
LY30 (Lysis at 30 Minutes)
What it measures: Percentage of clot lysis 30 minutes after MA
Reflects: Fibrinolysis
Normal Range: 0–8%
Interpretation/Intervention:
Clinical Use Cases in ECMO
TEG is particularly helpful in:
Pediatrics – where small changes in volume have significant impacts
Liver disease – complex balance between bleeding and clotting
Massive transfusion protocols – guiding FFP, cryoprecipitate, platelets, or antifibrinolytics
ECMO – when conventional labs don’t explain bleeding or clotting tendencies
Heparinase-Modified TEG: Differentiating Heparin Effect from Coagulopathy
In patients receiving heparin therapy, interpreting coagulation status can be challenging. Standard TEG may show prolonged R times due to heparin's anticoagulant effect, potentially masking underlying coagulopathies. Heparinase-modified TEG addresses this by neutralizing heparin in the blood sample, allowing for accurate assessment of the patient's intrinsic coagulation function.
When to Use Heparinase TEG
Consider heparinase-modified TEG in the following scenarios:
Post-Cardiopulmonary Bypass (CPB): To assess residual heparin effect and guide protamine reversal.
Liver Transplantation: To evaluate coagulation status in the presence of endogenous heparin-like substances released during reperfusion.
ECMO Management: To distinguish between heparin-induced anticoagulation and other coagulopathies.
Unexplained Bleeding: When standard TEG shows prolonged R time, and heparin effect is suspected.
Performing Heparinase TEG
Heparinase TEG is conducted by running two assays simultaneously:
Standard TEG: Measures coagulation parameters in the presence of heparin.
Heparinase TEG: Measures coagulation parameters after neutralizing heparin with heparinase.
Comparing these results helps determine if prolonged clotting times are due to heparin or an underlying coagulopathy.
Interpreting Results
Prolonged R Time in Standard TEG, Normal R Time in Heparinase TEG: Indicates heparin effect.
Prolonged R Time in Both Assays: Suggests a coagulopathy unrelated to heparin.
This differentiation is crucial for guiding appropriate treatment, such as administering protamine for heparin reversal or providing specific blood products for coagulopathy management.
Should a Standard TEG Be Performed Simultaneously?
Yes, conducting both standard and heparinase TEG assays concurrently is essential. This dual approach allows for a direct comparison, facilitating accurate identification of heparin's role in any observed coagulopathy.
Final Thought
Most of us learned labs like INR and aPTT in school, but ECMO patients live in a different world. Their coagulation status is a moving target, and TEG is one of the only tools that lets you watch that target shift in real time. TEG should always be interpreted in the clinical context—trends over time are more important than isolated results, and normal ranges may vary by institution or patient population. When considering interventions, always address the underlying cause and clinical scenario before transfusing blood products. For those working internationally, note that ROTEM is a similar tool with some different parameters but the same core principle. Whether you’re adjusting blood products, titrating heparin, or trying to figure out why your patient is bleeding (or clotting) despite “normal” labs, TEG is a practical game changer. Once you learn how to read the curve, you’ll never want to go back to relying solely on traditional lab tests.
AI and My ECMO Learning Journey
AI plays a significant role in how I research, understand, and communicate complex ECMO topics. From analyzing source materials to organizing ideas and generating podcast outlines, AI helps me stay curious and keep learning, so I can continue sharing insights with you.
Explore More:
lifesupport.training – Resources for ECMO and other professionals
ecmo.life – Information for ECMO patients and their loved ones
Occasional podcasts: youtube.com/@ecmo-143
LinkedIn Newsletter: ECMO 143: AI-Assisted Journey
Custom GPTs I Created:
AI ECMO Expert – A custom GPT designed to assist with ECMO research and education.
Micro Definitions (MD-GPT) – A custom GPT providing concise definitions for medical terminology.
Disclaimer:
This article is for educational purposes only and reflects the author’s understanding and interpretation of available guidelines, literature, and bedside learning. It does not constitute medical advice or represent institutional protocols. Always consult your ECMO team and local policies when making clinical decisions.
References:
Extracorporeal Life Support Organization (ELSO). Extracorporeal Life Support: The ELSO Red Book. 6th ed. Ann Arbor, MI; 2023.
ELSO. ECMO Specialist Training Manual. 4th ed. Ann Arbor, MI; 2022.
DellaVolpe J. The ECMO Book. San Antonio, TX: The Institute for Extracorporeal Life Support; 2024.
All TEG tracings were created using MS PowerPoint.