VV ECMO Part 2 of 3: Understanding and Managing Recirculation in VV ECMO
Recirculation in VV ECMO
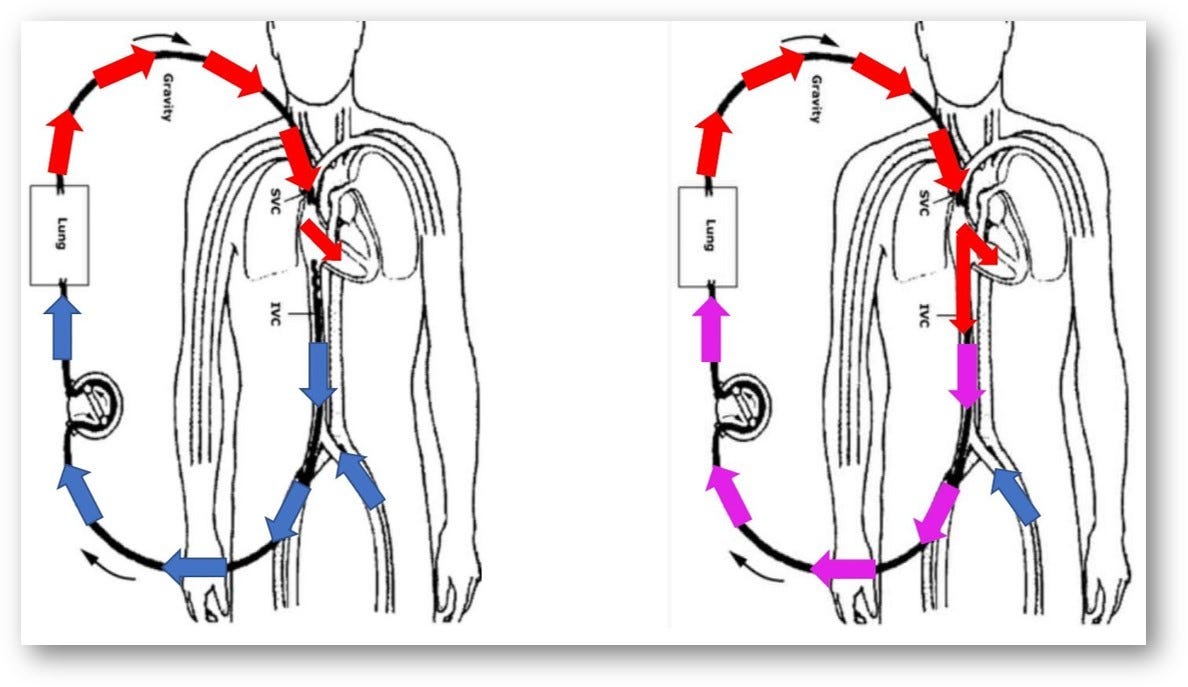
When I was a novice ECMO Specialist, I was taught that venovenous (VV) ECMO recirculation occurs when oxygenated blood from the ECMO circuit is drawn back into the drainage cannula instead of delivered to the systemic circulation. This reduces the efficiency of the ECMO circuit by reoxygenating already oxygenated blood, thereby diminishing the amount of oxygenated blood available to the patient’s body. Recirculation needs to be looked at but is not always emergent. It can provide valuable information about cannulation, ECMO flow, hemodynamic status, and shunt fraction (cardiac output vs. ECMO flow). However, it can become emergent due to a change in hemodynamic status or a shift in cannula position. As an ECMO specialist, being aware of the bigger picture is essential. Among many other things, ECMO specialists must be aware of sudden changes in ECMO pressures, Saturations, Cannula positions, or hemodynamic parameters. We check our ECMO patients at least hourly.
Causes of Recirculation
Cannula Positioning: Oxygenated blood is re-aspirated when the return and drainage cannulas are too close.
High ECMO Flow Rates: Excessively high flow rates can cause turbulence and mixing of oxygenated and deoxygenated blood, increasing recirculation risk.
Patient Anatomy and Physiology: Anatomical variations, such as vessel size and flow patterns, can predispose to recirculation.
Identifying Recirculation
Pre- and Post-Oxygenator Saturations: High pre-oxygenator saturation (>70-80%) and a smaller-than-expected difference between pre- and post-oxygenator saturations suggest significant recirculation.
Systemic Oxygenation (SpO2): Stable SpO2, despite high pre-oxygenator saturation, indicates circuit inefficiency.
Blood Gas Analysis: Regular measurements from pre- and post-oxygenator sites can reveal high pre-oxygenator pO2 or saturation, indicating recirculation.
Ultrasound or Echocardiography: Imaging can visualize blood flow patterns and cannula positions, identifying turbulent flow or cannula proximity issues.
Flow and Pressure Monitoring: Monitoring ECMO circuit pressures and flow rates for unexpected changes can signal recirculation.
How to Manage a VV ECMO Patient Experiencing Recirculation
Handling recirculation in a VV ECMO patient requires a systematic approach to optimizing cannula positioning, adjusting ECMO settings, and ensuring efficient oxygen delivery and carbon dioxide removal.
Assess and Confirm Recirculation: Regularly compare pre-oxygenator and post-oxygenator blood gases and monitor for clinical signs of inadequate systemic oxygenation.
Optimize Cannula Positioning: Use imaging to verify the position of the drainage and return cannulas, ensuring adequate separation to minimize recirculation.
Adjust ECMO Flow Rates: Consider reducing the ECMO flow rate to decrease shear stress and recirculation while ensuring adequate oxygen delivery.
Modify Sweep Gas Settings: Adjust the sweep gas flow rate to optimize CO2 removal.
Evaluate and Manage Hemodynamics: Monitor blood pressure, heart rate, and central venous pressure (CVP) to ensure hemodynamic stability.
Use of Dual-Lumen Cannulas: Consider switching to a dual-lumen cannula to reduce recirculation.
Regular Monitoring and Adjustments: Assess the patient’s oxygenation, ventilation, and hemodynamic status regularly to guide adjustments.
Alternative Cannula Configurations: In situations where a dual-lumen cannula is not feasible or effective, the sources suggest exploring alternative configurations, such as using two drainage cannulas to achieve bicaval drainage, to minimize recirculation

Four Interesting Considerations with Recirculation in VV ECMO
1. SpO2 as an Indicator
Good SpO2 levels suggest effective systemic oxygen delivery, even if recirculation is present. This means that the ECMO circuit compensates for any inefficiencies caused by recirculation.
Comparing Scenarios:
Scenario 1:
Pre-Oxygenator Saturation: 90% (indicating recirculation)
Post-Oxygenator Saturation: 98%
SpO2: 95%
Scenario 2:
SvO2: 70% (indicating less or no recirculation)
Post-Oxygenator Saturation: 98%
SpO2: 95%
In both scenarios, the oxygen delivery to the patient remains effective if the SpO2 is maintained at a reasonable level. Thus, focusing on SpO2 helps ensure that recirculation does not significantly impair oxygen delivery.
2. Reasons to Reduce ECMO Flow Despite Good SpO2
Reducing Shear Stress and Hemolysis: Higher flows increase shear stress on red blood cells, leading to hemolysis and elevated levels of plasma-free hemoglobin (PFHb).
Enhancing Circuit Efficiency: Significant recirculation means much of the ECMO flow is reoxygenating already oxygenated blood, which is inefficient.
3. Impact of Recirculation on pCO2 Levels
Based on my understanding, but not tested or seen, is that recirculation in VV ECMO can impact the blood’s partial carbon dioxide (pCO2) pressure levels. Recirculated blood that has been oxygenated and had its CO2 removed by the ECMO oxygenator re-enters the circuit with lower pCO2. This makes the oxygenator’s job of removing CO2 more efficient, continuously recycling and reducing systemic pCO2 levels.
Monitor Blood Gases: Regular monitoring of arterial and venous blood gases is crucial to assess CO2 removal.
Adjust Sweep Gas Flow: The oxygenator’s sweep gas flow rate can be adjusted to fine-tune CO2 removal.
Again, this is my belief, and I did not find any sources to confirm this information. Based on my understanding, this is a theoretical possibility, but it should be treated as speculation rather than fact. Further research and expert validation would be necessary to confirm or refute this hypothesis. Please comment if you have experienced this or not.
4. Drawing a Mixed Venous Blood Gas in VV ECMO Patients
I initially thought that using the distal port of the pulmonary artery catheter, like in other settings, would provide accurate mixed venous blood gas measurements. However, I learned that sampling from the distal port of a Swan-Ganz catheter in VV ECMO would give a reading similar to SaO2, not a mixed venous blood gas because the ECMO oxygenator acts as a surrogate lung. Instead, drawing from a central venous catheter (CVC) is more accurate.
Use a Central Venous Catheter (CVC): Ensure placement in a central vein and draw blood to measure central venous oxygen saturation (ScvO2). Avoid placing the CVC tip too close to the ECMO return cannula to reduce the likelihood of sampling recirculated oxygenated blood.
So, to sum it all up for ECMO Novices
When someone is a novice ECMO specialist, understanding recirculation in VV ECMO is crucial for providing optimal patient care. While recirculation can present challenges, it's important to remember that it's a manageable aspect of ECMO therapy. By regularly monitoring key indicators such as pre- and post-oxygenator saturations, SpO2 levels, and blood gases, you can effectively identify and address recirculation issues.
Remember that your role involves a holistic approach to patient care. This includes optimizing cannula positioning, adjusting ECMO flow rates and sweep gas settings, and maintaining hemodynamic stability. Like me, you will gain experience and become more adept at interpreting the interplay between recirculation, oxygenation, and CO2 removal.
Always stay curious and open to learning, as the field of ECMO is continually evolving. When faced with complex situations, don't hesitate to consult with more experienced colleagues. Your dedication to understanding these nuances will contribute significantly to improving patient outcomes and advancing your expertise in ECMO management.
If you have anything to add or comment on, please leave a comment. Hit the Subscribe button to receive notifications of new posts.
References:
Extracorporeal Life Support: The ELSO Red Book, 6th Edition. Published by the Extracorporeal Life Support Organization (ELSO), this comprehensive text is a key resource for understanding the principles and practices of ECMO.
ECMO Specialist Training Manual, 4th Edition. This manual provides in-depth training protocols and guidelines for ECMO specialists, covering cannulation techniques, patient management, and emergency procedures.
Various Other Source Materials. Additional insights and guidelines on ECMO practice, including hospital patient care practices.
Note: This article reflects my learning journey in ECMO and is intended for educational purposes only. It should not be used as a substitute for professional medical advice or guidance. Always consult with qualified healthcare professionals for clinical decisions and patient care.
Share and Subscribe. Join the ECMO 143 Learning Journey:
Other Links:
Follow me on LinkedIn: Jonathan B. Jung, RRT-NPS
Follow me on X (Twitter) “ECMO 143-Stay Uptodate” List on X
Acknowledgments:
I developed three custom GPTs, “AI ECMO Expert,” “ECMO Specialist Handover Practice,” and “Micro Definitions (MD-GPT),” for specialized research. These tools draw primarily from the ELSO Redbook (6th Edition), the ELSO Specialist Training Manual (4th Edition), various research papers, and articles. Additional research was supported by GPT-4o/o1, Claude 3.5 Sonnet/Opus, and Perplexity. Editing was performed with Grammarly. A.I. images and charts were created using Leonardo AI, DALL-E3 AI Image Generator, Microsoft Designer, and Adobe Express. Content for all articles sourced from Extracorporeal Life Support: The ELSO Red Book, 6th Edition, and ECMO Specialist Training Manual, 4th Edition.


