The RIDDLER Syndrome: A New Twist on Differential Gas Exchange in V-A ECMO

🔑Key Points
RIDDLER Syndrome refers to a CO₂ mismatch during peripheral V-A ECMO—when CO₂-rich ECMO blood perfuses the brainstem, causing tachypnea even though ABGs may look “normal.”
The right radial ABG can mislead you—showing low PaCO₂ while the brainstem is actually seeing high CO₂ from the ECMO circuit.
This syndrome underscores the importance of post-oxygenator ABGs and considering regional aspects of gas delivery, rather than focusing solely on systemic approaches.
I’m a novice ECMO specialist. I didn’t come into this job with all the answers—but I came with curiosity and a willingness to learn. I’ve been fortunate enough to land in a workplace full of smart, experienced people who have been generous with their time and guidance.
I use AI to help me read, research, and write about what I’m learning. This article is another step in that journey. I don’t write these posts as an expert—just as someone trying to understand ECMO better, one concept at a time.
This week, I came across a new syndrome described in Circulation, which helped me think differently about the role of CO₂ in V-A ECMO patients…
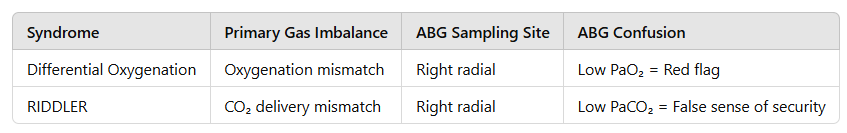
We’re used to hearing about Differential Oxygenation (a.k.a. North-South syndrome) in V-A ECMO—when the upper body receives poorly oxygenated native cardiac output, and the lower body is perfused by well-oxygenated ECMO blood. However, a new article in Circulation introduces a novel angle that caught my attention: RIDDLER Syndrome, also known as East-West Syndrome. Here is a breakdown of the Circulation article.
Why call it RIDDLER Syndrome?
The title of the article is a masterpiece of academic maximalism:
“Relatively Increased CO₂ Delivered to the Brain From the Descending Aorta Leading to an Elevated Respiratory Rate Causing Differential Hypocapnia (RIDDLER or East-West Syndrome): New Pitfalls in Awake Peripheral V-A ECMO.”
I looked everywhere trying to figure out what RIDDLER stood for—scanned the article top to bottom, hunted through references, chased blog posts, Reddit threads, anything. Nothing. Just endless recycling of the same title. No explanation. No acronym breakdown. No decoder ring.
After a long night of overcaffeinated searching… it hit me.
The RIDDLE was literally the title.
No, seriously. It’s just the first letters of the words.
R — Relatively
I — Increased
D — Delivered
D — Descending
L — Leading
E — Elevated
R — Respiratory
That’s it. That’s the whole thing.
Someone, somewhere, looked at that word avalanche and decided—correctly—that it spelled RIDDLER, and then just walked away like it was the most normal thing in the world. And honestly? I respect it.
It's ridiculous.
It's genius.
It's ridiculously genius.
And now I’ll never forget it.
The RIDDLE… has been solved.
Why RIDDLER Syndrome Matters
In awake, spontaneously breathing patients on peripheral V-A ECMO, we can inadvertently create a CO₂ imbalance across the brain—one hemisphere receiving decarboxylated blood from the lungs, the other hypercapnic blood from the circuit. This can trick us into making the wrong adjustments.
The Setup: How RIDDLER Happens
Here’s the six-step cascade:
Tachypnea develops (pain, exertion, sepsis, etc.), which increases native lung CO₂ clearance.
Right arm ABG shows a low PaCO₂ and high pH—looks like we’re over-sweeping.
Clinicians reduce ECMO sweep, expecting less CO₂ clearance.
But retrograde ECMO blood becomes more hypercapnic, perfusing the left brain via the left carotid artery.
Brainstem chemoreceptors detect rising CO₂ → further increase in respiratory drive → worsening tachypnea.
We respond to the wrong signal—the low PaCO₂ in the right radial artery—and drop the sweep even more.

You can see where this is going. It’s a vicious cycle, where right arm blood gases falsely reassure us, while the left hemisphere (and respiratory centers) are drowning in CO₂.
This isn’t just a theoretical issue—it led to reintubation in a patient with myocarditis on ECPELLA (ECMO+Impella) support.
Differential Oxygenation vs. RIDDLER: Know the Difference
How to Avoid the Trap
Don’t rely solely on the right radial ABG—it’s giving you only half the story.
Check post-oxygenator CO₂ to verify circuit decarboxylation.
Consider left radial or central venous gas sampling for a more complete picture.
Watch for inappropriate tachypnea that doesn’t respond to sedation or pain control.
Don’t reflexively reduce sweep gas just because of low PaCO₂ in the right arm—context is key.
Break the Cycle
Match sweep to blood flow (e.g., 1:1 ratio) once stable.
Aim for physiologic post-oxygenator pH and CO₂ targets.
Treat underlying causes of tachypnea: pain, anxiety, sepsis.
Consider gentle re-sedation, noninvasive support, or even reintubation in severe cases.
Final Thought
RIDDLER Syndrome is differential decarboxylation, requiring a shift in our thinking—especially in awake, peripheral V-A ECMO patients.
Don’t be fooled by the right radial blood gas.
I’ll admit—I hadn’t thought of CO₂ delivery as a regional issue until a previous article, Case Study: Refractory Metabolic Alkalosis, by guest editors Dr. Felipe de Andrade Arnaud and Dr. Jeffrey M. Scott. While pCO2 is the issue in both cases, the increased pCO2 in the case study was leading to increased refractory HCO3. We’re learning that gas exchange on ECMO isn’t just about oxygen anymore. It's about context, anatomy, and staying humble enough to say: “What’s going on here?”
📝 Note: This article is for educational purposes only and is not a substitute for professional medical advice. Always consult with qualified healthcare professionals for clinical decisions and patient care.
🚀 Join the ECMO 143 Learning Journey
Enjoyed this? Subscribe to my free newsletter, ECMO 143: AI-Assisted Journey, on LinkedIn, where I share ongoing insights as I learn and grow in the world of ECMO and critical care.
🌐You’re already on lifesupport.training—home of ECMO 143. Stay tuned for premium content including ELSO exam prep and critical care resources (ACLS, PALS, BLS, ATLS).
📺 YouTube Channel
🏢 Company Page
💬 Facebook Page
🧠 Acknowledgments
I created this article using a mix of AI-assisted research and curiosity-driven study. I’ve built two custom GPTs to help me dig deeper:
• AI ECMO Expert
• Micro Definitions (MD-GPT)
Special thanks to:
OpenEvidence · GPT-4o/o1 · Claude 3.5 · Perplexity · Gemini 2.5 · Storm (Stanford) · Grammarly · Leonardo AI · DALL·E3 · Microsoft Designer · Adobe Express
📖 Reference
Jung, C., Wengenmayer, T., & Duerschmied, D. (2025). Relatively Increased CO₂ Delivered to the Brain From the Descending Aorta Leading to an Elevated Respiratory Rate Causing Differential Hypocapnia. Circulation, 151(4), 289–291.
👉 https://doi.org/10.1161/CIRCULATIONAHA.124.071524